Ahhhh, my hands have thawed out enough to operate a keyboard in the new permafrost habitats of winter season dentistry. Thanks to the requirement for open window ventilation and fallows, through fervent shivering I’ve shifted the weight gained during the first lockdown.
We’ve been seeing patients from the moment we were permitted to open our doors. The initial approach was cautious to maintain social distancing. Opening more surgeries was an expansionary approach to correctly balance patient and staff safety.
As a large NHS practice, the hefty volume of patients requiring emergency or non-urgent treatment is slowly reducing. Yet we forever seem to be lying at the foot of the mountain to meet all patient needs.
At the start, the slower pace to the usual NHS flow felt great. We got to spend time with our patients, have that extra couple of minutes for the local anaesthetic to really sink in, and keep them comfortable instead of whizzing through treatments. We even had time to drink our tea while it was hot and thoroughly chew, instead of inhale, lunch.
Nurses had tranquil surgery turnaround time without queues of patients. I had time to do admin and referrals during working hours as opposed to my free time during lunch breaks or the end of the day. I believe GPs have scheduled admin time in their working week, a luxury to us dentists.
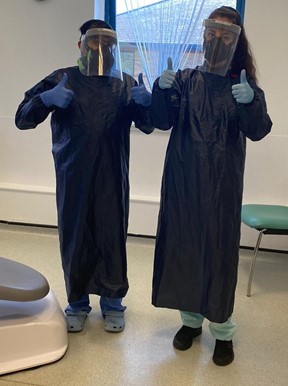
The SOP and extra PPE took a couple of weeks to get used to but it looks here to stay. Many patients are sympathetic of the PPE we don. I look forward to eventually ditching my perfected Darth Vader impersonation.
I can understand the enhanced protection of FFP3 masks, and we already wore eye protection and gloves as standard PPE. But could someone please explain the benefits of a plastic apron during non-AGP procedures. I feel like I’m walking around dressed to make sandwiches in a café.
My washing machine has taken quite the battering. I don’t think there’s ever been a time it went through so much use. I won’t miss the increased carbon footprint from the additional energy use and the plastic waste. Nor will I miss the image of the Death Eaters using my home as a hideout.

Our local area had some spare vaccine doses going. We only found out through word of mouth via local dental networks. Many of our practice got jabbed on Christmas Eve. So, if anyone asked, I told them I got a dead arm for Christmas. Second doses are rescheduled although it won’t bring an end to current working patterns.
Triaging patients did feel a bit of a pointless exercise, especially once all practices were able to see patients directly. Patients need care. Dentistry is not a work-from-home career. Plus, that routine of going out to work with regular social contact is keeping me sane.
It seems the NHS approach of fast-thrills dentistry has shot itself in the foot. Performance-based contracts, practice utilisation and access are only a few of many issues that spring to mind. Issues foretold in a world before COVID-19, further exacerbated by COVID-19.
The demise of NHS dentistry has long been prophesised. The current wide varying formula for contracting never suited all practices. Case proven with the new SOP which is a no-blanket approach and needs adapting as each practice requires. I personally don’t know any dentist that’s wilfully trying to do as little as possible.
Some practices have been able to attend to more patient needs than others. This isn’t because of gamesmanship as some have publicly outcried. It’s simply to do with the needs of the patient demographics that each practice serves.
High-needs practices will predictably have high levels of treatment, leaving less openings for routine care, especially once 30-minute fallow times are factored in. Low-needs practices may be able to resume routine care sooner.
Incidences of self-isolation are causing disruption to patient care. Some unfortunate practices have even had to close from outbreaks within the ranks. Each lost surgery day means having to play catch-up to hit those magic numbers once more.
In any event, UDAs are still the common denominator. Nothing else seems to matter about what you offer or how you go about doing it. Simply performance. Surely there must be another way to measure how practices are functioning.
In this game of stick or twist, the NHS has decided to stick with the same metrics. Some practices may be tiring of the cards they’re holding and decide to chance their luck. Can the NHS afford to let practices take that twist?
About Hussein Hassanali
Hussein graduated from the University of Liverpool in 2009 and completed his PG Dip in Restorative Dentistry in 2020 which granted Fellowship of BAARID. He is an NHS Associate Dentist in York with a special interest in ultrasonic restorative dentistry. He has a broad range of experience having worked in both NHS and private, and both corporate and independent practices. To date, he has over 20 publications to his name and continues to support the profession through his regular contributions, as well as being on the BDJ Reader Panel and an Editorial Advisory Board Member of Young Dentist Magazine.